Per the CDC, a sharps injury is a penetrating stab wound from a needle, scalpel, or another sharp object that may result in exposure to blood or other body fluids. This can include scalpels, razors, needles, lancets, blades, broken glass or any other sharp implement.
The CDC knows there are many needle sticks and sharps injuries that occur during a year in hospitals and healthcare facilities, with over half of them unreported. Most happen innocently, like when nurses are caring for patients, or when a needle is being recapped with two hands. What risks do these injuries pose, and what’s the best way to treat and avoid them?
What to Do If You Experience a Sharps Injury
First, don’t panic. Know that it’s OK. Most needlesticks, splashes, and sharps injuries do not result in the transmission of any worrisome infections, so take a deep breath. This situation usually turns out just fine if you follow up, as needed, with a medical provider.
There were 58 known workplace transmission of HIV and 150 suspected cases of HIV due to workplace exposures. It’s important to follow up with medical care immediately if there has been an exposure.
If you have just had a needlestick or a sharps injury:
- Wash the needlestick site or site of injury with soap and water
- Report what happened to your supervisor, if this occurred while on the job
- Seek medical treatment immediately
If you’ve been splashed with blood or a body fluid:
- Wash splashes to any abrasions, cuts, or non-intact skin with soap and water
- Flush splashes to the eyes with clean water, saline (mild salt water), or sterile eyewash irrigants
- Flush splashes to the nose or mouth with water
- Wash off any other body fluids that have splashed on you
- Report what happened to your supervisor, if this occurred while on the job
- Seek medical treatment immediately for any splashes to the face (eyes, mouth, nose) or on non-intact skin (cuts, abrasions, puncture wounds, sores, burns).
Splashes to intact skin should be washed off, but without splashing mucus membranes (mouth, nose, eyes, etc.) or non-intact skin (cuts, abrasions, sores, burns). This probably poses no risk for major blood-borne illnesses, but please follow safety protocols where you work and check with a medical professional about any exposures.
Why Do You Need to Immediately Seek Medical Treatment?
There are certain diseases like HIV, Hepatitis B, and Hepatitis C that can spread through blood exposure and it’s important to take any steps immediately to reduce the risk of transmission. Post-exposure prophylaxis refers to medication or other interventions that can reduce the chance of developing a disease after being exposed to an infection. This can mean a daily medication for HIV, or a vaccination and immunoglobulin injection for Hepatitis B.
For HIV exposure, these drugs only need to be taken for 4 weeks (28 days). But it’s important that this daily treatment is started as soon as possible. You need to start the drugs within 72 hours, but better yet within the first 24 hours of being stuck.
Medical clinicians in the US can call the Clinicians’ Post Exposure Prophylaxis (PEP) Line at 1-888-448-4911for help.
Post-exposure prophylaxis can also be used after someone has been exposed to the infection through rape or through consensual sexual activity.
Do All Splashes and Needlesticks Need Treatment?
Always wash away any body fluids and clean any needlesticks or other injuries, but talk to your healthcare provider about whether you actually need treatment. If the needle or sharp has not been used on anyone else, it won’t, of course, transmit any infections from anyone else. An injury though can always become infected like any other injury so it’s important to keep any injury clean.
If, on the other hand, the needle to sharp had been used on someone else, the source patient (whose blood was on the needle) could transmit infection. But if the person does not have any infections that you might be concerned about, you may not be at risk for anything in particular. This is something you should talk about with a healthcare professional to help understand what risks you may or may not face.
If you’re a healthcare provider, you may know whether the patient had HIV, Hep B, or Hep C. Depending on the laws and regulations, there may be a way to quickly find out if the source patient is infected with any of these viruses. This will depend on where you are and what the exposure was. Please talk to your healthcare provider about this.
Likewise, not all body fluids transmit all infections.
HIV is transmitted by:
- Blood
- Amniotic Fluid
- Semen and pre-seminal fluid
- Rectal fluids
- Vaginal fluid
- Breast milk
HIV can also be transmitted by fluids that would only be reached by a needle or scalpel during a medical procedure:
- Cerebrospinal fluid
- Pleural fluid (that builds up around the lungs)
- Synovial fluid (from within joints)
- Ascites or Peritoneal fluid (from inside the abdomen)
- Pericardial fluid (that builds up around the heart)
However, other fluids would normally have to have blood present to transmit HIV. The risk of HIV transmission is very low, without blood, from:
- Urine
- Spit
- Saliva
- Sputum
- Sweat
- Tears
- Feces
- Nasal Secretions
- Vomit
This means that being spit on is not a risk factor for HIV. Likewise, being scratched also doesn’t spread HIV if there is no contact with HIV+ blood.
HIV is also not spread through swimming, the air, mosquitoes, hugging, sharing toilets, sharing food or drinks. Likewise, although Hepatitis B virus can be found in saliva and spit, it is not believed to be spread through kissing or sharing utensils, per the CDC.
Also, the good news is that needles do not remain infectious for long. An old needle, long abandoned on the street, is unlikely to be a risk, but do talk to your healthcare provider about each exposure.
Are Only Nurses at Risk?
Most Needlesticks and Sharps Injuries affect nurses and doctors. However, some injuries affect those who are not medical professionals. It’s important to always stay safe when there are needles, scalpels, or blades around.2
Centers of Disease Control and Prevention. HIV and Occupational Exposure.
A child may try to reach into an overfilled sharps box to pick up a shiny needle. A groundskeeper in a park may be pricked by a needle left on the ground. A police officer or a corrections officer may be injured by someone with a bloody needle or knife. Someone else may worry about their risk because their spouse is a nurse who has had a needlestick. Similar exposures can occur in the home with razors, blades, and even a needle used for a splinter. This can also happen, in rare cases, if a tattoo parlor or a nail salon does not follow necessary safety regulations. There are lots of ways that these sorts of injuries can affect all of us, so seek medical advice if there’s any concern for exposure.
In some places, health facilities are not in line with Infection Prevention and Control. This is one reason for the spread of Hepatitis C worldwide. There are times when needles are reused. Sometimes IV fluids or IV tubing are reused. Other times reusable devices are not fully decontaminated between usages. In other cases, needles are used after patient use to obtain more medications from a shared reusable medicine container. Reuse of needles in any form after use in a patient can lead to spreading infections.
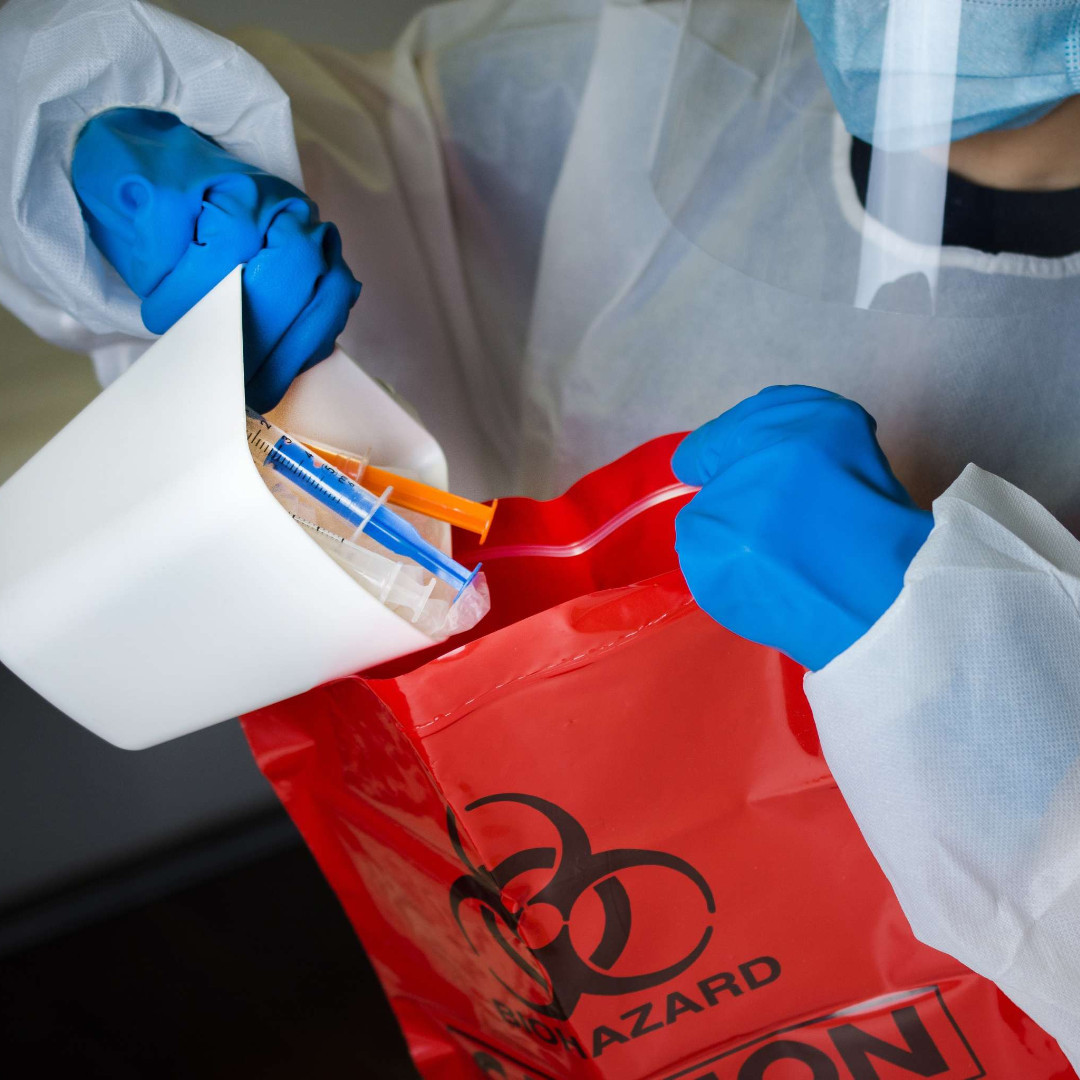
What You Can Do to Prevent Needlesticks or Sharps Injuries
It’s about being prepared.
- Train in safe needle use
- Avoid using needles when not necessary
- Ensure enough rest when working with needles
- Avoid recapping needles
- Use only one hand with a needle
- Do not rush
- Do not walk with a used needle
- Do not hand a needle to someone else
- Have a proper workspace
- Dispose of needles in a sharps disposal box
- Discard sharps disposal box before it is full
- Never reach into a sharps disposal box
- Use needles with safety devices
- Use safety blades and razors
- Avoid using glass when plastic could work
- Consistently use the same type of needle
- Report any needlesticks immediately to an employer
- Look for risks for needlesticks
- Determine why any needlesticks have happened
Just to be on the safe side, don’t use needles unless you know what you’re doing and you need to. There’s a risk in using a needle. Every time you use one it can risk a needlestick. It can also create more risks for the patient (who can always get an infection and pain at the site of the injection). In general, only use needles when well trained to do so and when it’s necessary.
This content, What to Do If You Experience a Sharps Injury, by Megan Coffee, MD originated on Very Well Health and was updated on February 09, 2022.