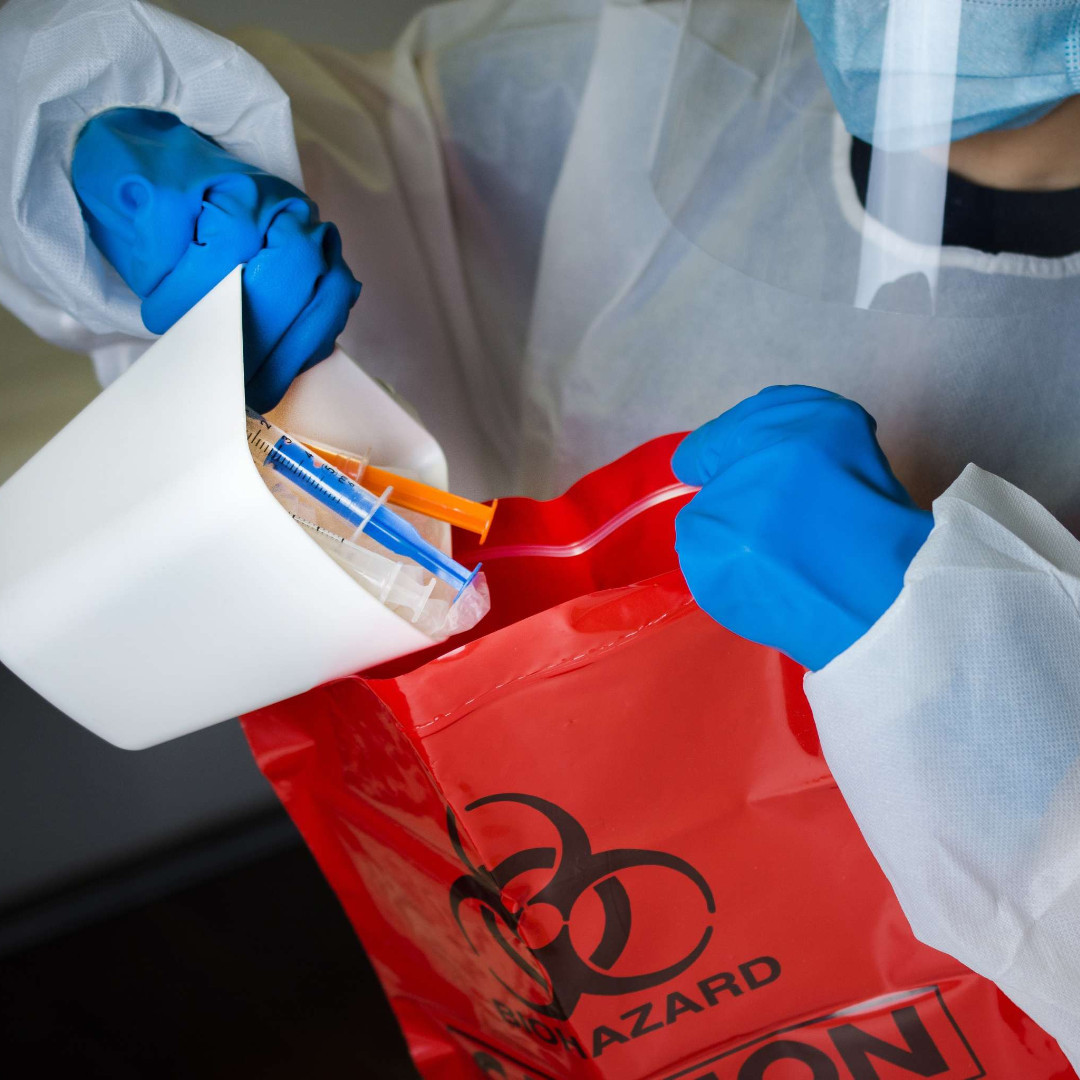
Pandemic pressures, alongside staff fatigue and stress, are the most likely causes of a “high incidence” of sharps injuries among nurses in the past year, a report from the Royal College of Nursing has suggested.
The fact that not all nurses have access to safer sharps or appropriate training and education could also be a contributing factor, said the report, which is based on responses from more than 7,500 RCN members.
The report, called Blood and Body Fluid Exposures in 2020, was written by an RCN working group that was led by a New Zealand-based consultant microbiologist, Terry Grimmond.
According to the survey results, during the their career, 96% of college members had experienced a blood and body fluid exposure risk and 63% had experienced a sharps injury.
Meanwhile, in the past year, 15% of respondents said they had experienced a sharps injury, up from 10% in the RCN’s 2008 survey on the same issues.
When this previous survey was commissioned, the RCN led a subsequent campaign for the safer use of needles in health and care settings.
In 2013, following its campaign, new safer sharps regulations were introduced to try to reduce sharps injuries.
The RCN commissioned the 2020 survey, which was carried out in November and December last year, to track what the situation was like now.
But the college said the latest findings suggested that there was “still some way to go to protect all parts of the nursing workforce”.
The survey also suggested that a quarter (25%) of mental health unit staff sustained sharps injuries in the last 12 months, as did 22% of care and nursing home staff, as well as 18% of nursing staff who worked in patients’ homes.
Meanwhile, 18% of acute staff had experienced a sharps injury in the past year, while 17% of general practice staff had the same.
In addition, the results revealed that more than a quarter of nursing staff (27%) felt fatigue was a contributing factor to their most recent sharps injury – the most popular reason cited.
More than one in 10 (12%) said staffing levels had contributed to their injury, while 25% cited a lack of safety equipment and 9% said the wearing of personal protective equipment (PPE) had been a factor.
A further 9% reported a lack of training and education, and 21% cited a lack of space.
Overall, the RCN said there was a concerning lack of training, as 25% of those surveyed said they had no training on safe sharps use and 21% had not received any education on reporting sharps injuries.
According to the report, at their last sharps injury, 35% of staff were using a safer sharp.
The report authors said the reason for the “high incidence” of sharps injuries in 2020 was “difficult to ascertain as the UK has little BBFE data available, however, it is likely related to Covid-19 workloads, fatigue, and stress”.
“That not all members have access to safer sharps, device training and BBFE education, may be a contributing factor to the high incidence, and also needs investigation to ascertain if reduced access is due to ‘not available from employer’ or ‘not taken up by employee’,” the report added.
Results also indicated that “preventative measures by employers are not protecting” nursing staff against BBFE, noted the authors.
Of those who experienced a sharps injury, 29% said it happened before a procedure, 26% during a procedure and 21% during disposal.
Meanwhile, 11% cited improper disposal, 8% said it happened after device activation and 5% during device activation. Almost half (49%) of injuries were with a sterile needle.
Concerningly, results also showed that after injury, less than half of respondents (48%) attended a follow-up meeting and 40% reported not receiving any medical advice.
A further 82% said they perceived the disease risk from sharps injuries as “low to nil”.
Jude Diggins, RCN interim director of nursing, policy and public affairs said: “These findings suggest the pandemic has highlighted a problem that has not been fully tackled yet.
“Most sharps injuries can be prevented and there are legal requirements on employers to take steps to prevent healthcare staff being exposed to infectious agents from sharps injuries.”
Rose Gallagher, RCN professional lead for infection prevention and control, added: “All nursing staff who work with sharps should have training in how to use them safely.
“In 2013 new regulations were brought in to reduce sharps injuries but these findings suggest there is still some way to go to protect all parts of the nursing workforce.”
She added: “We now need to see greater efforts for better reporting and training to not only prevent injuries but to ensure there are stronger procedures to follow-up and protect nursing staff after injuries.”
The report closed with a list of recommendations including calls on organisations to review sharps injuries data and prevention policies annually, while evaluating with users the safest sharps devices available.
It also recommended that semi-auto or auto safety-mechanism devices should be adopted where appropriate and that all standard devices should be removed from an organisation once they were replaced by safer devices.
This post was first shared on Nursing Times, ‘Still some way to go’ to protect nurses from sharps injuries, warns RCN, on May 21, 2021.