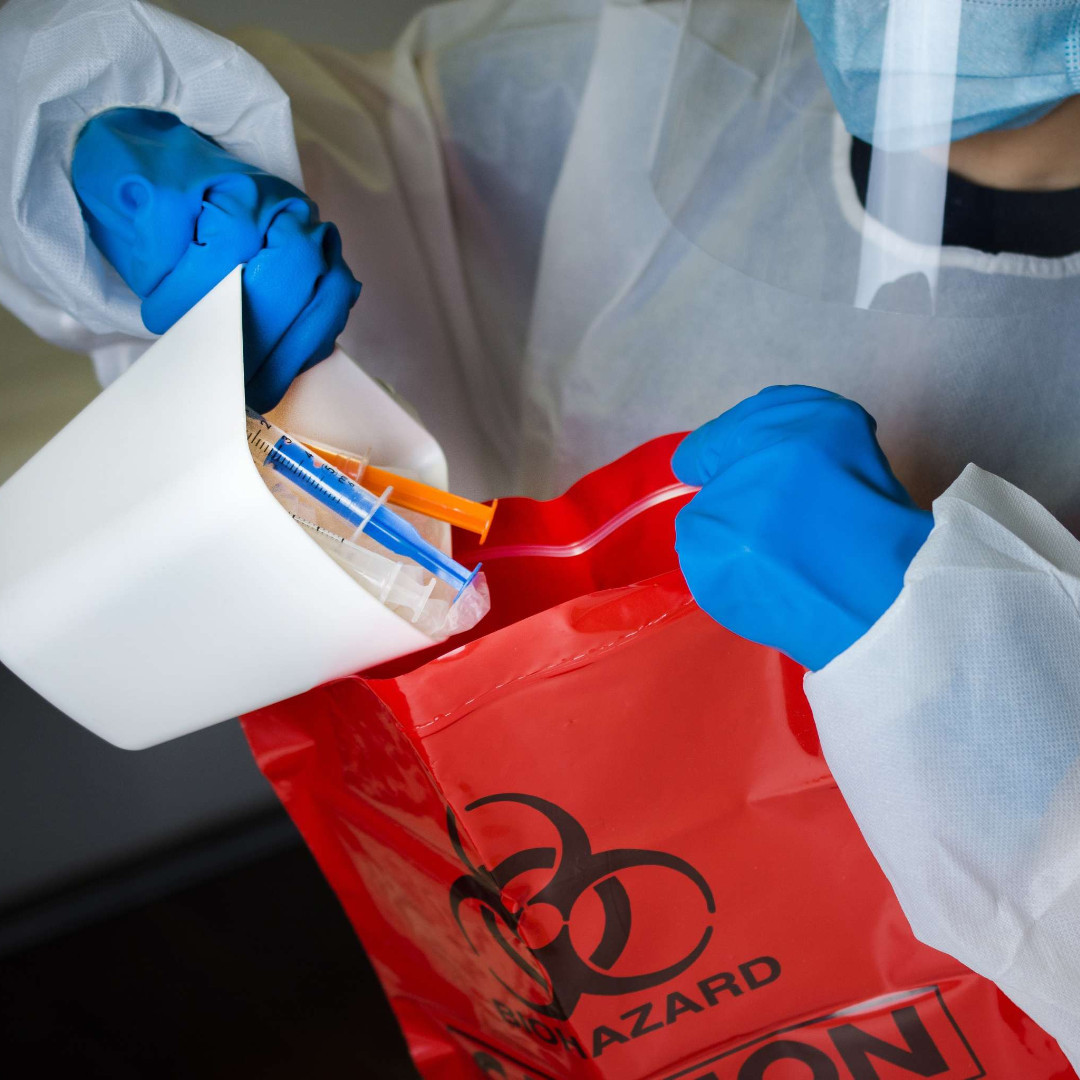
The increase in the need for personal protective equipment (PPE) and its use during the COVID-19 pandemic has produced a rise in medical waste as institutions dispose of gowns, gloves, masks, face shields and shoe covers that have been exposed to the virus.
“There definitely is more regulated medical waste being generated, and a lot of it is derived from PPE,” said Rudy Vingris, the health care business development manager at Waste Management Sustainability Services. The challenge, he noted, “is that there isn’t a national standard that applies across the board to determining what types of COVID-19–related PPE should be regulated as medical waste. It’s up to individual states.’
The Occupational Safety and Health Administration and the CDC released guidance specific to COVID-19 waste, which determined that the virus is a Category B infectious substance. This means PPE and other medical waste generated in the treatment of patients with COVID-19 can be managed in the same way as other waste related to Category B infectious substances, in contrast to the more hazardous Category A infectious waste generated in the management of diseases such as Ebola.
“This classification means that, unless the PPE is grossly contaminated with blood or bodily fluids to the extent it could lead to an infection, it is technically just trash and can go to the solid waste stream,” Vingris said.
However, given that COVID-19 is a highly communicable disease, treating exposed PPE as ordinary waste rather than hazardous medical waste gives some people pause. “The University of Nebraska Medical Center has done studies on surface and air contamination associated with the virus, and has found measurable concentrations in the air and on surfaces where patients have been,” said Fred Massoomi, PharmD, the senior director at Visante (Sci Rep 2020;10[1]:12732). “We know this is a virus that likes to linger. So, while some systems are managing COVID-related PPE as routine waste, others are treating it as biohazard waste that gets autoclaved or incinerated, depending on how they classify it.”
Clues From the States
Many states have issued their own guidance statements on managing PPE exposed to the coronavirus. New Jersey, for example, clarifies that “PPE and cleaning materials (e.g., wipes, rags) contaminated with blood, excretion, exudates, or secretions from humans who have COVID-19 are considered regulated medical waste,” whereas materials that are not contaminated in that way can be disposed of as ordinary waste.
California allows for some discretion in its regulations on PPE: “If the facility determines that any PPE should be disposed of [as solid waste], used gloves, face masks, coveralls, etc., should be placed in a lined container, preferably with a lid/cover. Tightly close off the bag before disposing the solid waste items into the … waste bin for pickup by the waste management company.”
Disposal of regulated medical waste is, of course, much more costly than solid waste. “It’s more expensive by probably an order of magnitude of 10 times or more, although not as expensive as something like RCRA [Resource Conservation and Recovery Act] waste that we would see in an oncology pharmacy,” Vingris said. “So is it breaking the budget? No, but it is definitely something that folks have had to adapt their planning and budget for as part of overall waste management.”
Furthermore, “as hospitals and pharmacies set up vaccination centers, they will also be generating even more waste that is definitely considered regulated medical waste, such as sharps containers. That is definitely going to drive up costs at these institutions.”
This post was first shared on Parmacy Practice News, Navigating PPE Waste Disposal During a Pandemic, on April 20, 2021.