Health system executives are finding it difficult to stay ahead of the multiple trends culminating at once—reimbursement pressures, rising drug costs, regulatory complexity (340B), and the central role of pharmacy in value-based care.
Ed Francis, a senior director of life sciences at West Monroe Partners, says changes in drug pricing represents a particularly important issue that health executives will need to watch out for in the coming year, starting with optimizing the drug rebate system.
“Congress and the executive branch have discussed everything from eliminating the system entirely to writing laws that increase pricing transparency,” he says. “Even without government intervention there has been movement with some new PBMs that offer rebates as 100% pass-through to consumer. Other companies have emerged that are offering online drug price comparisons in a local area. All of this will help to solve the problem.”
Here are five other policies to keep an eye on in the year ahead.
1. USP 800
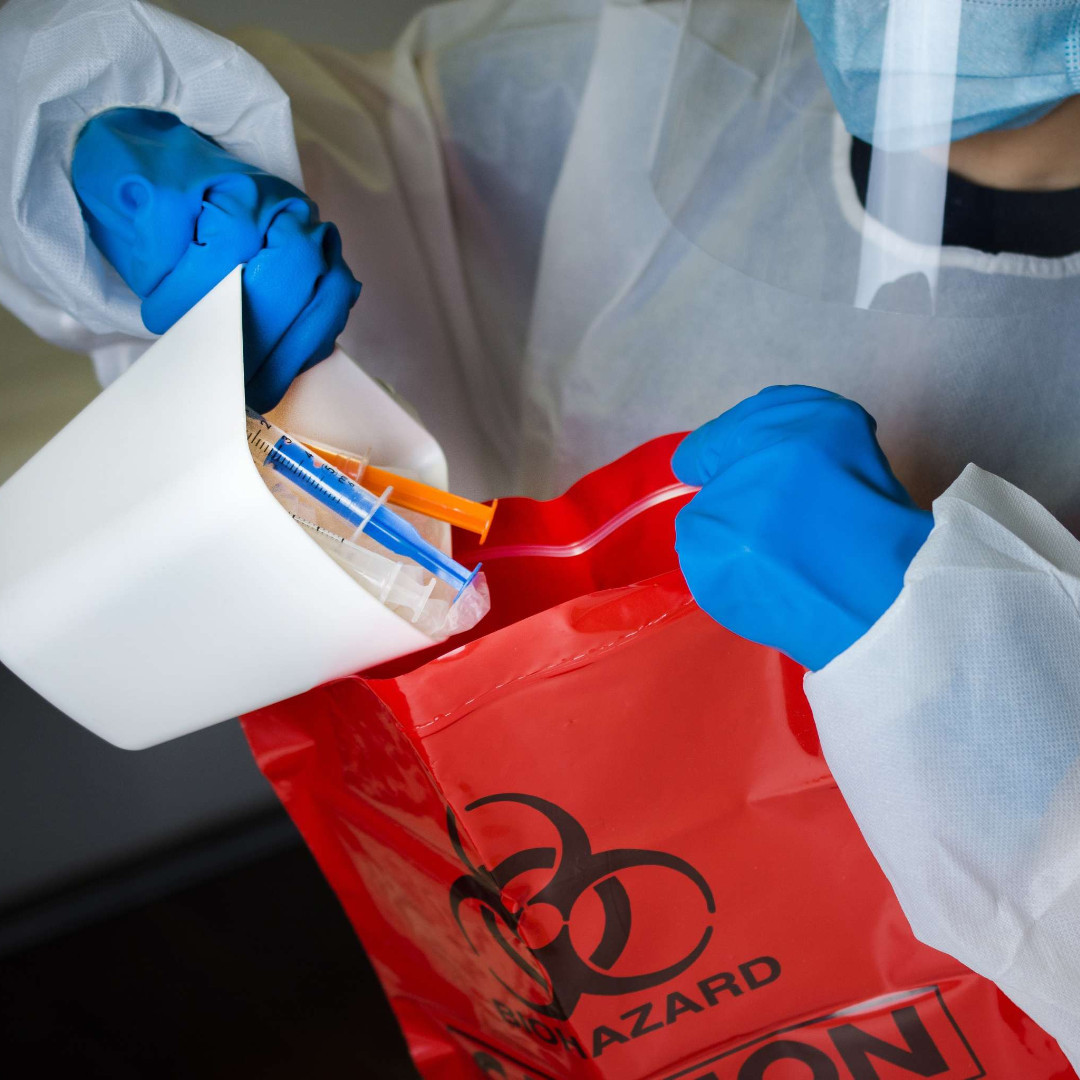
Pharmacy expert Ernie Gates, president of Gates Healthcare Associates, believes that compliance with USP 800—the new workplace safety standard for pharmacy—will bedevil many healthcare organizations and the cost of non-compliance could be staggering.
USP 800 is about protecting the healthcare worker, patient, and environment from accidental exposure to hazardous drugs and requires changes to standard operating procedures across an organization, beginning with receipt of a hazardous drug and ending with disposal.
“Many pharmacies, including those inside of institutions such as hospitals, are not prepared to comply with USP 800, which goes into effect later this year,” he says. “This could be problematic for any healthcare organization that is dependent upon pharmacies, including health plans that operate or simply reimburse pharmacies.”
2. Drug Supply Chain Security Act (DSCSA)
The DSCSA was designed so an electronic system could track and trace certain prescription drugs in the United States. Katrina Harper, senior clinical manager, pharmacy for Vizient, says what’s important with DSCSA is compliance with current regulations to ensure the integrity of the pharmaceutical within the supply chain.
“We are now starting to see enforcement actions in the form of fines,” she says. “One large wholesale distributor was the FDA’s first ever warning letter for non-compliance. They also need to be preparing to comply with the new aspects of this regulation that take effect in 2020.”
By 2020, all Rx products covered under DSCSA must be serialized, and all transactions can only involve serialized product.
3. The Lowest Price Act
This act was signed into law on October 10, 2018 and will become effective either on or after January 1, 2020. Brian Romig, director at Navigant, says it blocks Medicare Advantage plan providers or providers of a Medicare Part D prescription drug plan from using gag clauses that prohibit pharmacists from alerting Medicare customers of differences between their insurance copay and what the patient would pay without using health insurance coverage.
“The act was implemented to increase price transparency for consumers covered under Medicare or Medicare Advantage,” he says. “Health system pharmacists can help patients find better pricing by advising that there are options available to them.”
4. EPA update of the Resource Conservation and Recovery Act (RCRA) standards
These regulations were published in early 2019 to clarify an organization’s responsibility related to the disposal of hazardous and controlled substance pharmaceuticals in the waste stream.
“The good news is that there will be improved alignment to DEA requirements for disposal and the change in requirements may impact an organization’s waste generation classification which could result in lower costs,” says Joyce Thomas, associate principle, pharmacy advisory services for Vizient.
5. CMS Hospital Outpatient Prospective Payment Proposed Rule CY 2019 (OPPS)
Romig explains this proposed rule further expands cuts to the 340B Drug Pricing program made in 2018 and institutes a site-neutrality payment policy for hospital outpatient departments by cutting reimbursement by 40% for the most commonly reimbursed G-codes in order to match payment under the Physician Fee Schedule.
“The proposed rule also includes a request for information related to a potential Competitive Acquisition Program for Part B drugs and biologics, which would run through the Center for Medicare and Medicaid Innovation,” he says.
6. Provider status changes
Expanding the scope of practice for pharmacists is being considered in state legislatures and in Congress. This is particularly true in states with large underserved areas.
“In Congress, a main consideration is whether Medicare should cover payments to pharmacists in these underserved areas,” Romig says. “More than half of the 100 total members in the U.S. Senate have signed on to support the Pharmacy and Medically Underserved Areas Enhancement Act [S 109). The bill has surpassed the number of votes necessary to pass this legislation in the Senate. The same bill is HR 592 in the House of Representatives.”
The bill would provide for Medicare coverage and payment for certain pharmacist services that are furnished by a pharmacist in a health-professional shortage area, and that would otherwise be covered under Medicare if furnished by a physician. On the state level, many are considering allowing pharmacists to prescribe oral contraceptives, while others would allow them to prescribe treatments for flu or strep throat. Virginia is considering allowing pharmacists to perform opioid abuse counseling. Pennsylvania is discussing allowing pharmacists to counsel for tobacco cessation.
The author, Keith Loria, is an award-winning journalist who has been writing for major newspapers and magazines for close to 20 years.
This post, Seven Pharmacy Regulations Health Execs Must Watch, first appeared on https://www.managedhealthcareexecutive.com.